Over one thousand miles from home, two VA-BC™s met to save a life.

After months of repeated line complications, April Winborne’s, MSN, APRN, FNP-C, CPUI, VA-BC™, patient was running out of options for chemotherapy infusions. He had an occluded central line with a suboptimal terminal tip location due to central venous stenosis. Formerly active in bow hunting and fishing, and now spending more time and effort on his infusions, he found his quality of life dwindling.
“The patient said, ‘If you can’t make this work for me, I’m done. I’m giving up, and I’m tired’,” Winborne recalled.
Winborne immediately began looking for alternative sites, but because of the small size of her hospital and limited resources, it was hard to determine the next steps.
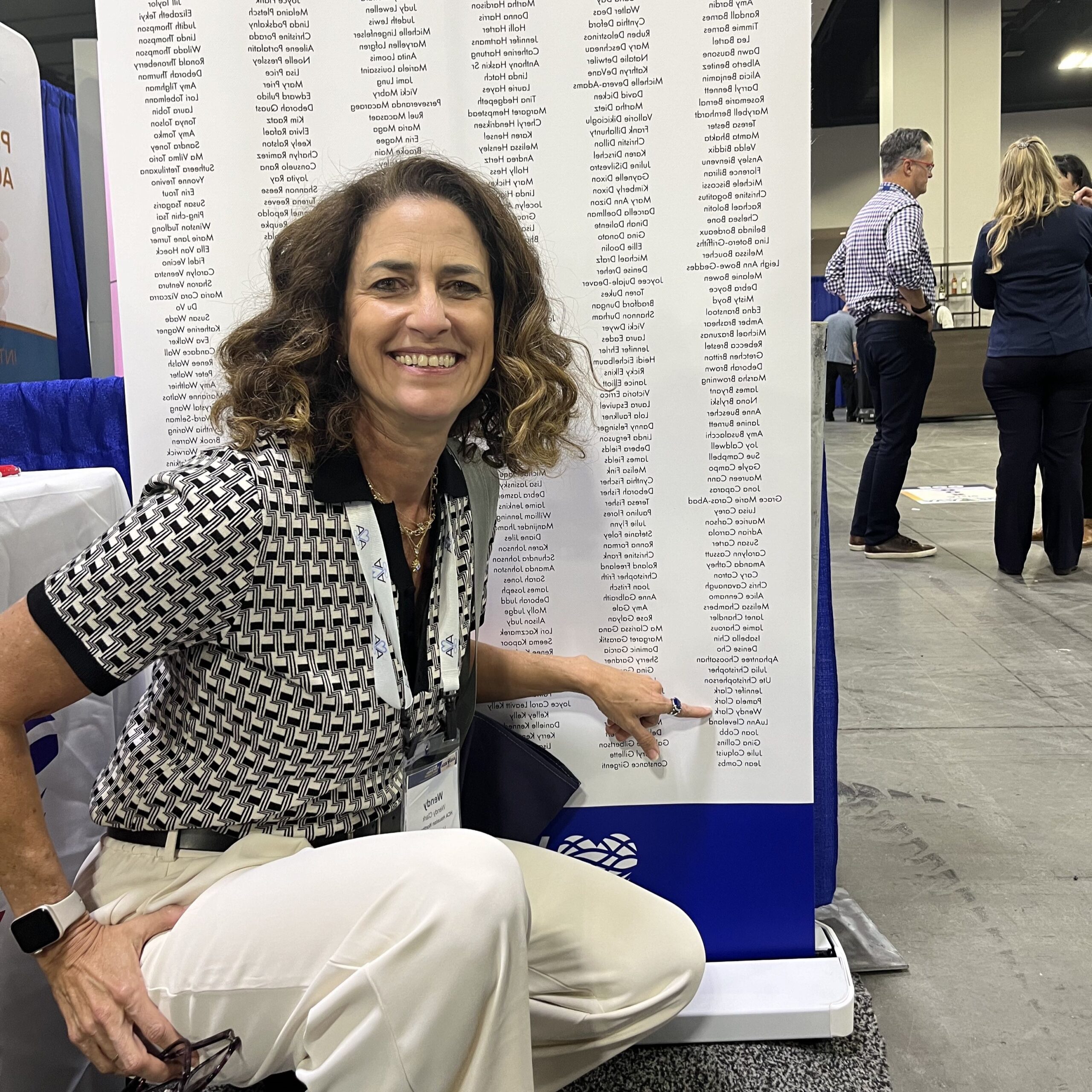
Luckily, Winborne had an in-person training with Matthew Ostroff, MSN, APRN, VA-BC™, at St Joseph’s University Hospital in New Jersey a few weeks later.
When they met, they discussed the care that a patient like Winborne’s would need. Ostroff recommended that the patient receive a catheter from the femoral approach, and since the patient is ambulatory and active, tunneling the catheter to the abdomen would allow him to take part in the activities he enjoys.
“I wasn’t going to let this patient down… I knew the resources and I knew how to make this happen.
Could we pull it all together? I didn’t know. I had to try.”
It’s a procedure that Winborne was familiar with but had never done herself. It was, however, Ostroff’s area of expertise. To Winborne’s surprise, Ostroff offered to travel to Louisiana to perform the procedure.
“It was like it was meant to be,” Winborne said, though Ostroff insists that Winborne creates her own luck.
“April sought out the knowledge,” he said. “She didn’t wait for someone to give it to her.”
Unfortunately, the two-person team could not get approval for Ostroff to conduct the procedure in Winborne’s hospital.
Traveling cross country to save a patient’s life
Refusing to give up, Winborne thought that if the patient was on board, she could bring him across the country to Ostroff.
 A week after Winborne finished her training with Ostroff, and the patient consulted with Dr. Howard Benn, an oncologist at St. Joseph’s University Hospital, Winborne was back on a plane to New Jersey. This time, with the patient and his wife.
A week after Winborne finished her training with Ostroff, and the patient consulted with Dr. Howard Benn, an oncologist at St. Joseph’s University Hospital, Winborne was back on a plane to New Jersey. This time, with the patient and his wife.
“I wasn’t going to let this patient down,” Winborne said. “I knew the resources and I knew how to make this happen. Could we pull it all together? I didn’t know. I had to try.”
Within an hour of arriving at the hospital, the patient had his new line.
Even months later, Winborne said it is the best line any of her patients have.
“As a vascular access specialist, we are always brought to the patient’s bedside to provide the appropriate intervention, but rarely does a patient come to us for that solution,” Ostroff said.
Bringing back the knowledge to rural hospitals
Throughout her time as Chief Nursing Officer in her organization, Winborne has seen the many ways that oncology patients approach their cancer journey. Still, she found that this patient inspired her.
“Sometimes I wonder why this is happening,” Winborne recalled the patient saying as they waited for the procedure. “Why I have cancer, why I’m being flown here to get this access to come back to Louisiana. Maybe it’s all so I can help somebody else.”
Ultimately, that was Winborne’s goal too: to bring this knowledge back to her hospital so she can help those who need alternative access sites.
Not only did Winborne coordinate the care with Ostroff and his institution’s oncologist, but she also helped ensure funding for the trip. Ostroff’s institution covered the procedure and the patient’s church raised money for the travel costs, while all other expenses were covered by a GoFundMe account that Windborne created.
“Sometimes I wonder why this is happening. Why I have cancer, why I’m being flown here to get this access.
Maybe it’s all so I can help somebody else.”
Moreover, Windborne used her own money—funds her father left her after he passed away.
“I never knew what to do with [the money], but he said I’d figure it out one day,” Winborne said.
“April went so far above and beyond what any clinician would do for their patient,” Ostroff said. “It just shows what kind of person she is. She’s just amazing.”
Ostroff and Winborne hope that more online or in-person training resources will be available in the coming years to provide education to smaller institutions like Winborne’s. With these resources, more clinicians may be able to think outside the box for patients that do not fit in it.