You are an experienced clinician, with a solid working knowledge of what you do and confidence in your ability to do your job. So, what’s next for your career? How do you know if an additional board certification is the right path for you?
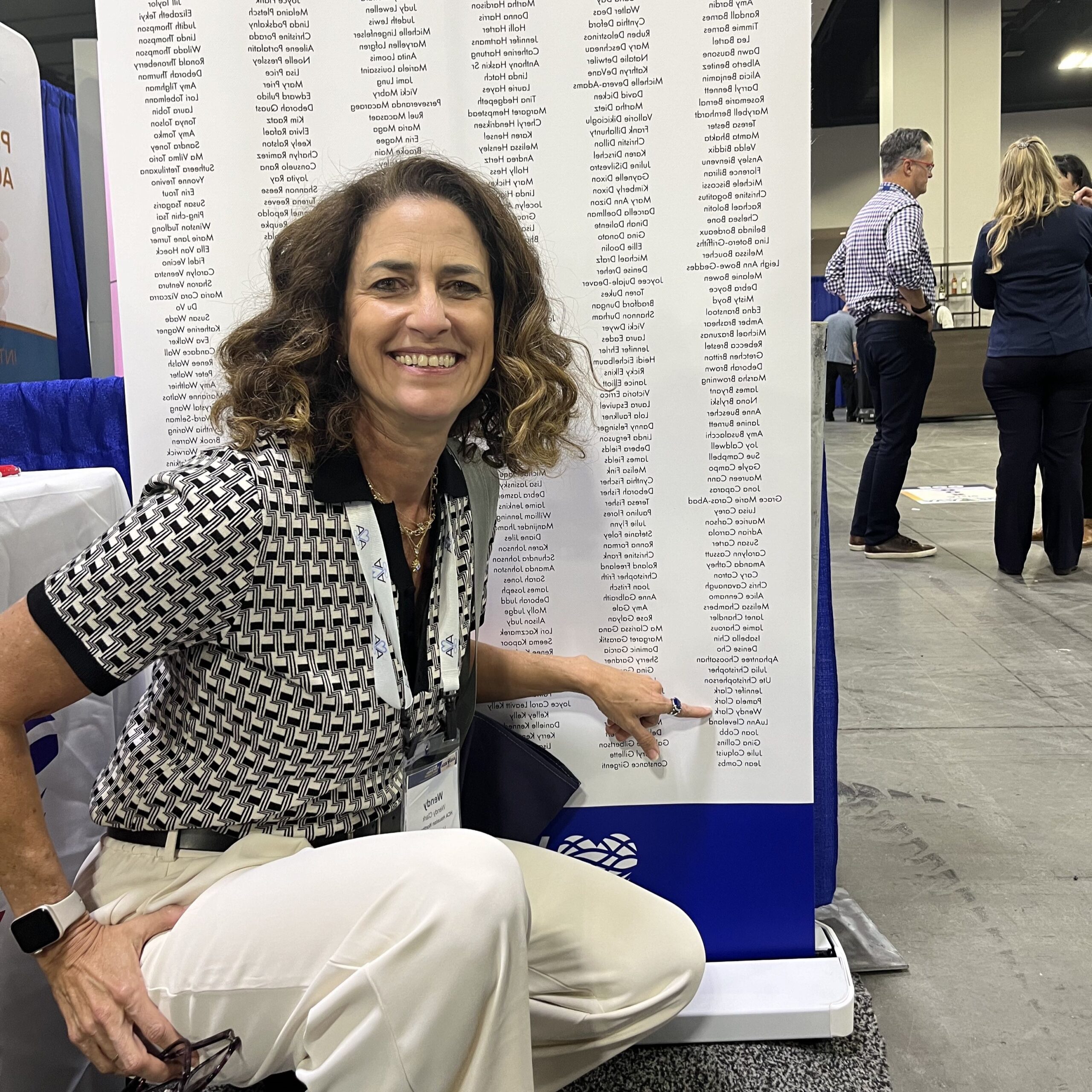
Chris Cavanaugh, MSN, RN, CRNI, VA-BC™, is a champion for continued education, both for herself and her fellow clinicians. She walks us through how she determined certification was in her future, and how to know if it’s in yours, too.

1. Consider your environment.
Chris Cavanaugh worked as a nurse for several years before gaining her first certification – the Certified Registered Nurse Infusion, or CRNI. Prior to that, she worked in the ICU, in radiology, and then in home infusion. It was there that she decided to set her sights on additional certifications.
Going into someone’s home to administer care was a personal setting to Cavanaugh. In a more vulnerable environment, she felt it was important to have a credential to show that she was competent in her care.
“That’s when I realized I really needed to be certified,” Cavanaugh says. “It gave an extra level of credibility to what I did and what I said.”
2. Evaluate your confidence in your work.
Cavanaugh advises that those looking to get certified in their specialty should have at least a year of experience. This allows time for the clinician to get exposure to different scenarios and be comfortable with their troubleshooting abilities. If you feel assured with your work most days, Cavanaugh says that this is a good sign that you are ready to start your certification journey.
Some certified clinicians find that their personal confidence increases once they gain an additional board certification. Because they have a deeper knowledge of the subject matter, they understand the rationale behind their care.
“It just shows an extra level of commitment that other nurses, they may be just as good technicians—but being certified means that you understand the theory, the ‘why,’ and you’re good at troubleshooting,” Cavanaugh says.
3. Assess your goals for your current job and your overall career.
Certification may also give clinicians a boost in later job opportunities. After adding CRNI to her name, Cavanaugh became a preceptor, an opportunity to which she attributes her certification. “I had that extra level of knowledge of what the standard of care really should be.”
Now, when hiring for her own team, she says she has more confidence in candidates that have additional certifications, including the Vascular Access-Board Certified™ (VA-BC™) credential.
“Being certified certainly looks better on a resume. It will certainly help your career.”
After transitioning to the industry side of vascular access, now a clinical education manger, she was among the first group of clinicians to sit for the VA-BC™ exam. Even though she had not worked directly with patients for some time, she remembered feeling relief and excitement for the credential. It is the only multidisciplinary credential specific to vascular access, and according to Cavanaugh, it was long awaited.
“I think it’s a professional obligation for us to understand best practices, and those best practices are constantly evolving,” she says. “Although vascular access has been around for a long time, we’re still learning new things all the time.”
She cites ultrasound guided IV insertions for example. Five years ago, she said, the option to use ultrasound to place a peripheral line was relatively unheard of. Now, it is becoming standard. Certification, she says, helps clinicians stay on top of these developments in technology and evidence-based care.
“I think we owe it to our patients to always provide the best practices,” she says. “If you’re not keeping current with [the] literature, and being certified drives you to do that, then you really are missing out – and your patients are missing out, more importantly.”
To see if vascular access board certification is for you, visit our information about the exam.